We make patients healthier and happier, and doctors less exhausted
Remove documentation burden from clinicians: our AI recognizes the dialogue, structures a medical note in your EHR, and monitors the quality of your clinicians’ work — with fewer clicks.
Documentation and the EHR take away the most valuable thing — human care for the patient
When clinicians are busy with forms, both speed and service quality suffer.
This increases the cost per visit, stretches queues, and reduces clinician presence in the conversation. Our AI assistant removes routine and returns focus to the patient.
- queues caused by documentation delays
- fragmented data and after-hours charting
- uneven note quality across clinicians
What clinics say
Selected feedback about Humarin rollout and the team’s work.
...First our providers ditched the notebooks and all the scratch-paper notes. Then visits started getting shorter — and we were seeing more and more patients every day...
...We’d already worked with a bunch of other AI vendors, but none of them ever offered to integrate the model into our EHR for free. You were the first ones to do that...
...Before you, we’d talked to all kinds of characters. You were the only team that really listened, took our needs seriously, and then turned around and integrated with our EHR...
...Over the last few months I’ve come to the conclusion that even a basic AI is already miles ahead of the average medical professional in our system...
...Honestly, it’s just been a lot nicer working with you. You’re actually willing to meet the client halfway and make things work...
...I always hear the same thing from our personnel: ‘We don’t want this, we can’t do this.’ Truth is, they just don’t want their mistakes on display — and the AI brings everything out into the open. Our chief medical officer asked me to roll out Humarin specifically so we’d finally see the whole picture...

Letter summarizing the Humarin.Transcribe pilot results.
Medical service lifecycle
From EHR documentation to quality control and real-time support — modules are mapped to each step.
Fill the EHR chart from the clinician–patient dialogue
Quality control of how the visit is conducted using the Calgary–Cambridge model
Form a diagnosis and treatment plan in line with Ministry of Health clinical guidelines
Validate diagnoses and treatment
Real-time help answering complex clinical questions
How Transcribe works
You can already reduce up to 70% of clinician time spent in the EHR. Clinicians talk — Transcribe charts
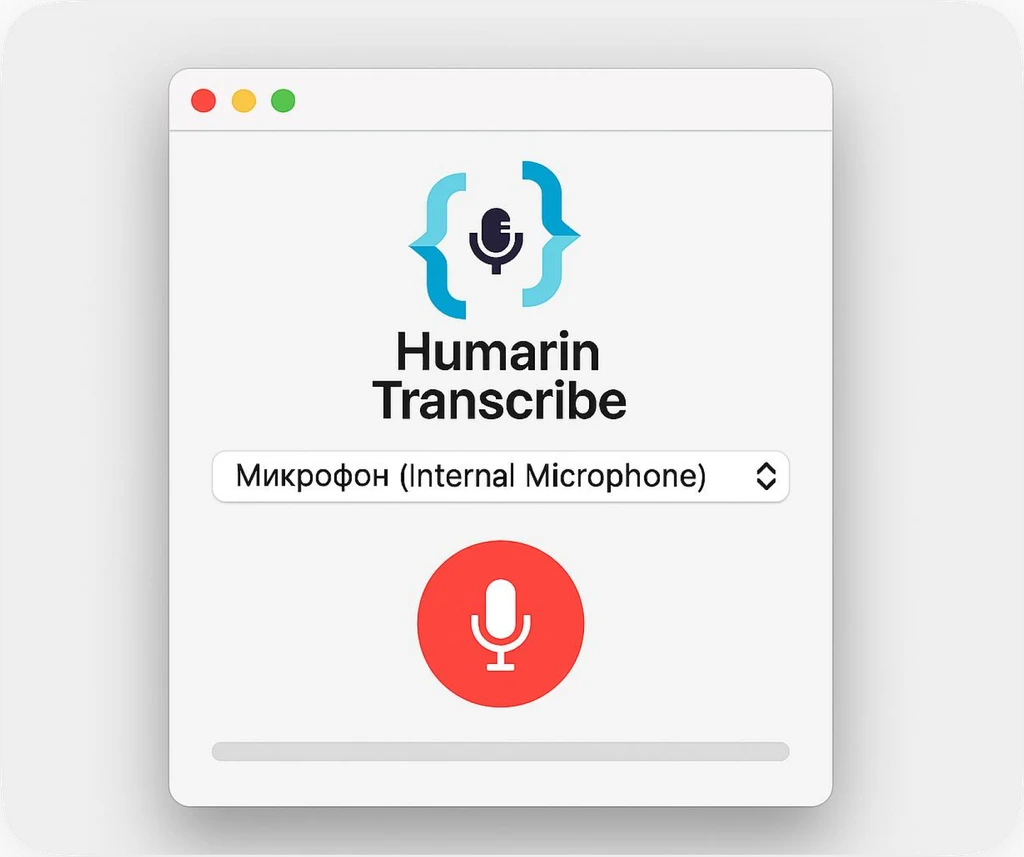
Transcribe understands medical context and fills EHR sections during the visit
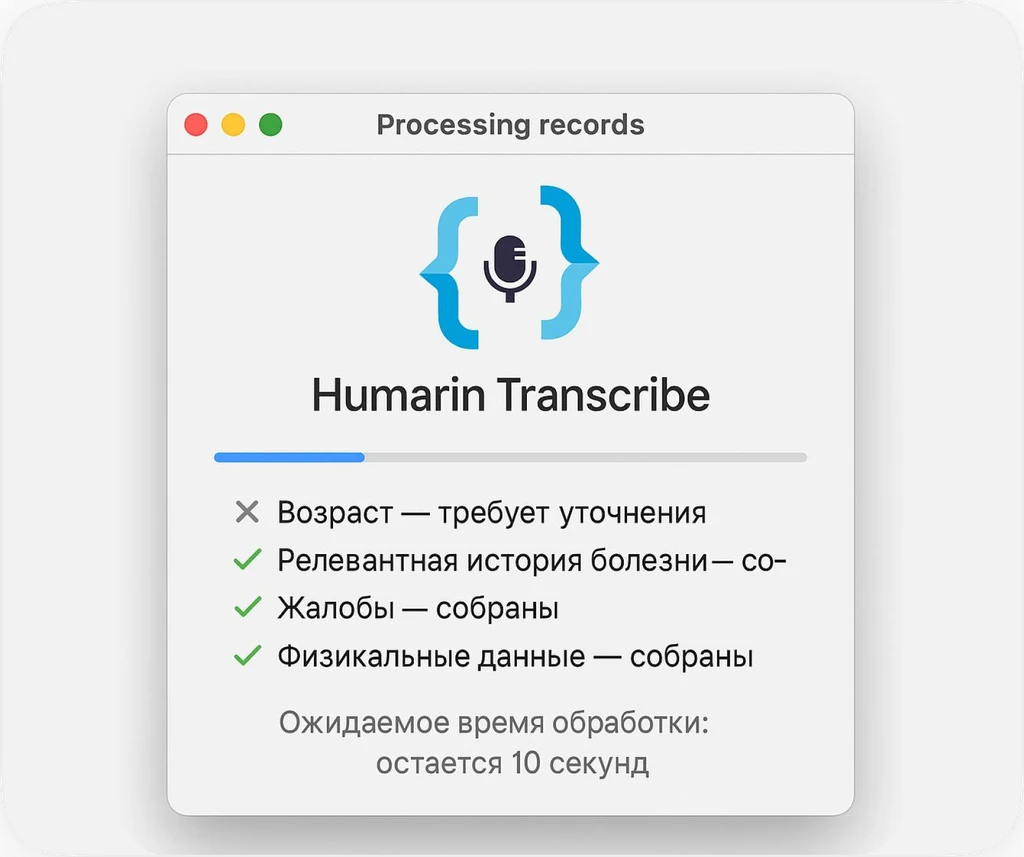
No mistakes or abbreviations — no need to switch attention away from the patient
No after-hours charting — the patient gets the clinician’s full attention
Want to see how much impact your healthcare system could unlock?
This is a rough estimate — real results depend on your clinic.
Request a demo
Leave your contact — we’ll show workflows, discuss integration, and outline a pilot for your clinic.
A short walk-through of the clinician journey: visit recording, structuring the note in the medical chart, review and manual edits, and seamless EHR integration.
- templates and scenarios for different specialties
- integration options (API/RPA)
- pilot plan, success criteria, and commercial pricing